PICC Lines – A Multifaceted Intravascular Therapy Device
Accounting for nearly 10 million deaths worldwide in 2020 alone, cancer remains one of the leading causes of death, and with the recent spread of Covid-19, cancer care has undoubtedly faced tremendous disruptions. Despite the advancement in cancer diagnostics technologies, and treatments, the instability arising from the pandemic has inflicted a major setback to the healthcare system.
The incidence of cancer amongst Covid-19 patients was observed at a rate of 6% with a much higher mortality rate than usual.[1]
More than 3/4th of the patients undergoing cancer treatment had experienced some delay in their treatment due to Covid-19.[2] However, to overcome this setback and minimize all the future ones, it is important to develop a robust healthcare eco-system by ensuring reliable access to medical devices and diagnostic technologies.
In the oncology field, Vascular Access Devices (VAD) is the go-to tool for doctors to deliver chemotherapy in cancer patients, by gaining easy access to their bloodstream. Typically, a VAD is recommended in patients requiring mid-term to long-term intravenous treatment involving recurring infusions of caustic drugs or hyperosmolar fluids in chemotherapy, TPN administration, blood sampling, infection, or acute pain therapies.
Despite multiple options available, the conventional IV catheters (or Peripheral Intravenous Catheters, PIV) are the most widely used tool for administering intravenous treatment.[3] In practicality, this preference has got less to do with PIV’s simplicity and inexpensiveness than lack of awareness of better alternatives amongst healthcare professionals.
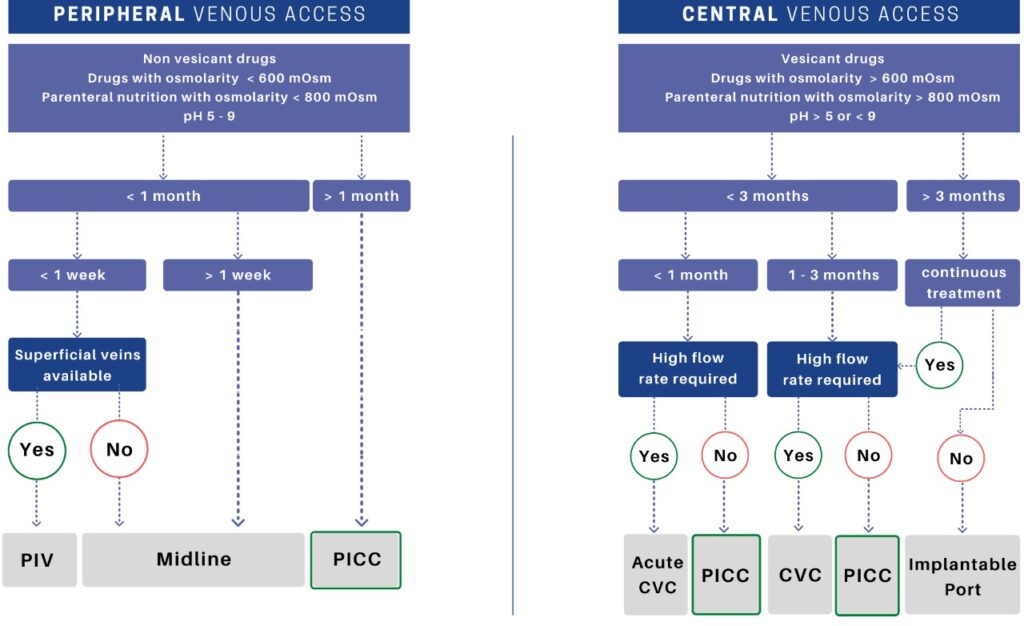
Different types of VAD available
A versatile tool for intravenous therapy – PICC lines (Peripherally Inserted Central Catheter)
As the name suggests, a peripherally inserted central catheter (PICC) is a long, thin, flexible tube inserted into one of the large peripheral veins of the upper arm and ends in the central vein (superior vena cava) of the heart. PICC lines can be utilized to obtain both peripheral venous access and central venous access for delivering intravascular therapies for usually a period of 1-3 months (or more).
Why choose a PICC line over the conventional PIV?
A PIV, commonly known as an IV cannula, is typically a short catheter, placed peripherally in the forearm that ends in the arm itself. When compared to a PICC line, the latter is sturdier, thicker, and longer, ending high up in the central vein.
The PICC has a higher dwell time of around 1-3 months (or sometimes even more) compared to short-term access of up to 96 hours in the case of PIVs. Therefore, delivery of intravenous therapy using a PICC line requires fewer needlesticks that not only decreases the economic burden on the hospital, but also the needle prick trauma on the patients, especially pediatric.
Multiple repeated cannulations pose serious complications like infections, quick depletion of the number of peripheral veins available, damage to veins, increased risk of mechanical phlebitis ad increased risk of local cutaneous complications. PICC lines allow greater mobility as no IV boards are required.
Moreover, high osmolarity infusates like chemotherapy drugs are too caustic to go through the smaller peripheral veins using regular PIVs.
When are PICC lines used?
A PICC line is a safe and reliable way to access the central vein
- For Reliable and Continuous IV access for 5 days or more.
- Administration of TPN (Hyperosmolar solution)s
- Continuous administration of chemically vesicant drugs that are known to cause peripheral phlebitis (inflammation)
- Patients with skin conditions like open chest wounds, burns, an existing tracheostomy
- Patients with GI disorders
Where is a PICC line inserted?
The smaller peripheral veins of the cardiovascular system are utilized for PICC line insertion to reach the larger central veins because they provide a safer route and a higher flow rate ensuring a better hemodilution of the drug.
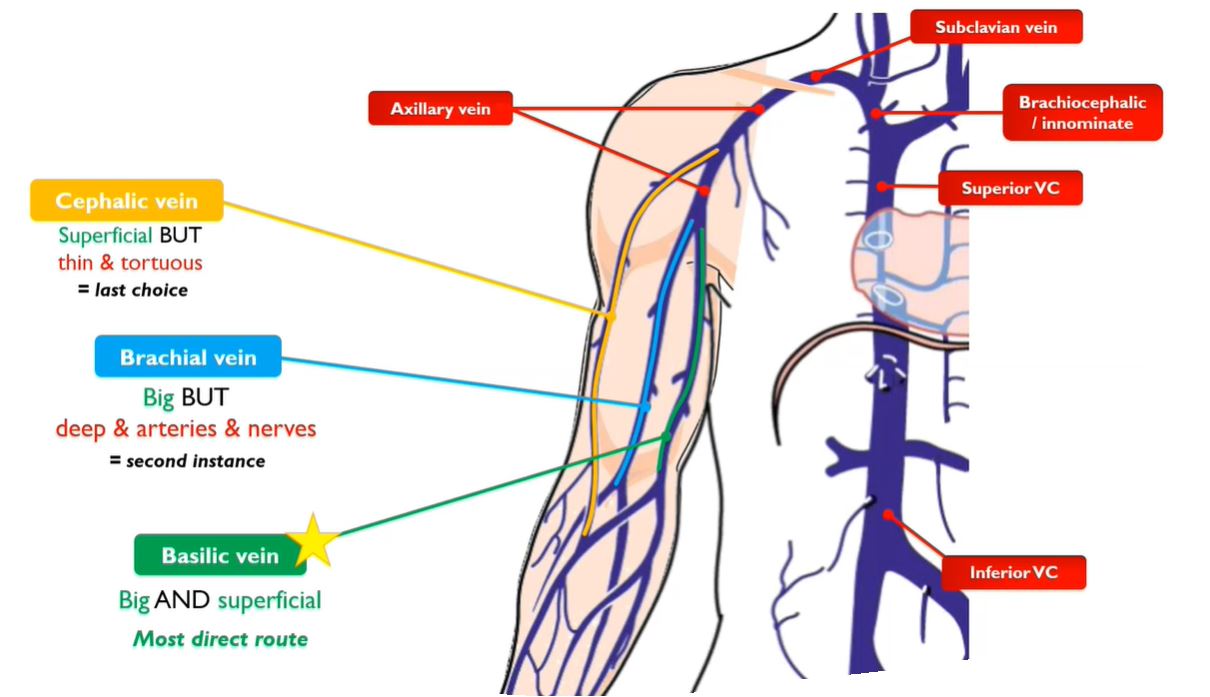
Different PICC insertion routes (amongst which the right basilic vein is the most preferred)
The tip of the PICC line ultimately terminates within the superior vena cava. More precisely put, the catheter tip location should be at the cavo-atrial junction level – approximately 1 or 2 vertebrates below the carina, for long-term therapy.
What is the recommended length?
In an average adult patient, the approximate length of the right and left sides of the PICC line should be 39cm and 45cm, respectively. However, the lengths are variable to the patient’s needs and the ideal length is best determined by the clinician. For cutting the PICC to the desired length, it is highly recommended to employ a proximal trimming technique instead of distal trimming to maintain the catheter tip integrity and minimize the chances of deep-vein thrombosis. [4]
What is the ideal dwell-time of PICC?
As long as the PICC line remains patent, infection-free, and in working condition, it can be left in place from several weeks to months, until the end of treatment. Having said that, Vygon usually recommends it for a period of 1 – 3 months (or sometimes even more) depending on the requirement and clinicians’ discretion.
Choosing the right VAD depending on the duration and frequency of therapy, patient’s needs, medical history, and preferences is a crucial step in delivering effective treatment to the right patient at the right time.
Improving cancer care goes beyond innovative treatments; it means ensuring existing interventions are available to those who need the most and the ability to obtain reliable venous access in the inpatient and outpatient setting is the first step in it.
Access to knowledge and healthcare services are the only way we can return the stability and bridge the inequities in cancer healthcare.
References: –
[1] Yang, Ludi et al. “Effects of cancer on patients with COVID-19: a systematic review and meta-analysis of 63,019 participants.” Cancer biology & medicine vol. 18,1 (2021): 298-307. doi:10.20892/j.issn.2095-3941.2020.0559
[2] Cancer Action Network, “The most commonly reported impact is a delay in care, with 78% of respondents reporting a delay to obtaining health care, up from 24% in the previous survey.”, American Cancer Society, 15 April 2020, p3
[3] Huang, LS. et al. “Current practices of peripheral intravenous catheter fixation in pediatric patients and factors influencing pediatric nurses’ knowledge, attitude and practice concerning peripheral intravenous catheter fixation: a cross-sectional study.” BMC Nurs 20, 236 (2021). https://doi.org/10.1186/s12912-021-00758-1
[4] Steele, Denise, and Colleen M. Norris. “Cutting peripherally inserted central catheters may lead to increased rates of catheter-related deep vein thrombosis.” Journal of Infusion Nursing 37.6 (2014): 466-472.








