What is the Role of Pulmonary Surfactant in Neonates?
Surfactant is a substance that reduces the surface tension at the interfaces of two liquids, between a gas and a liquid or between a liquid and a solid. Detergents, soaps, paints, adhesives, motor oils, etc are all examples of commonly used surfactants in daily life. Now, another such lesser talked about surfactant is the one naturally occurring in the alveoli of human lungs – pulmonary surfactant, preventing alveoli from collapsing.
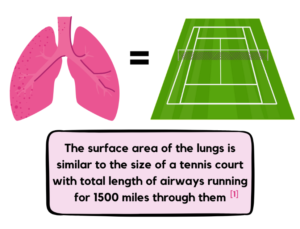 The respiratory system is the system that tirelessly works to help us breathe, comprising an integrated network of lungs, bronchi, bronchioles, pharynx, larynx, nose, and mouth.
The respiratory system is the system that tirelessly works to help us breathe, comprising an integrated network of lungs, bronchi, bronchioles, pharynx, larynx, nose, and mouth.
The basic fundamental unit of the respiratory system is the alveoli, where the main exchange of oxygen and carbon dioxide takes place between the lungs and the blood. The alveoli are tiny, hollow cup-shaped air sacs making up the entirety of the lungs, having very thin walls surrounded by many blood capillaries.
The mean total number of alveoli in an adult human being is 480million located at the end of the bronchioles. [2]
Now, these alveolar walls have a thin layer of water lining their inner surfaces which are formed when water vapor condenses during gas exchange while breathing and this water film creates a strong force at their surface, called surface tension; an intrinsic property of the water molecules to pull each other together to form a sphere (as water tends to form drops). So, it would naturally lead to collapsing of the alveoli into a sphere, ultimately causing problems in breathing.
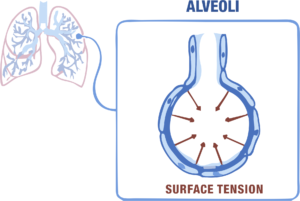
According to Laplace’s Law, the pressure that facilitates the lungs’ collapse is directly proportional to surface tension and inversely proportional to the alveolar radius.
[P = 2T/r]
where P = pressure on alveolus, T = surface tension, r = alveolar radius
This implies the smaller the radius the higher will be the collapsing pressure and vice-versa; and as alveoli are small in radius to promote a higher surface area to volume ratio in the lungs, they would have a much higher collapsing pressure.
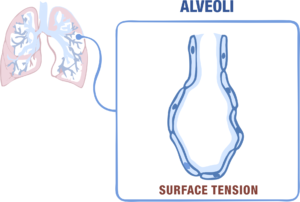
To counteract this high surface tension, our body provides an easy fix. The alveolar type II cells of the lungs secrete a phospholipoprotein fluid, pulmonary surfactant, that lowers the surface tension at this air-water interface and keeps the alveoli wide open to allow efficient breathing, whilst maintaining the structural integrity of alveoli.
Role of pulmonary surfactant
- Reduces collapsing pressure of alveoli, and ultimately the lungs
- Provides high compliance to allow the lungs to expand and extend to accommodate more air
- Regulates the sizes of different alveoli providing stability
- Provides immune protection from infectious agents like bacteria, etc
Surfactant Production and Consequent Complications in Neonate
Fetal lung development starts from the 3rd -17th week of gestation and continues 1 – 3 years postnatally. The surfactant production first begins and is detectable in the amino fluid between the weeks 25 – 36 (until birth) [3] [4]
However, usually before 32 weeks of gestation, the fetal lungs are immature and underdeveloped and birth before this progressively increases the chances of respiratory
difficulties due to lack of surfactant and respiratory alveoli. [4] Therefore, preterm infants are at a greater risk of developing morbidities, the most common being Neonatal Respiratory Distress Syndrome, which can lead to hypoxia and other serious complications.
In Europe, RDS is observed for about 90% of babies born at 24wks of gestation and for 80% of babies born at 28wks of gestation. [5]
Babies born 6wks or more before term completion require supplemental oxygen for the different strategies. This includes antenatal corticosteroid administration to the mother, assisted ventilation, and exogenous surfactant administration, which drastically enhanced the preterm survival rates by 1995. [6] [7]
Surfactant Administration Strategy
 Vygon offers a trailblazing solution, Surfcath, a thin, flexible catheter for surfactant administration using the advanced LISA method (Less Invasive Surfactant Administration) while maintaining non-invasive ventilation, thus reducing the unpleasant effects on the tiny baby. This LISA method is gradually replacing the traumatic antecedent procedures using an endotracheal tube and INSURE method.
Vygon offers a trailblazing solution, Surfcath, a thin, flexible catheter for surfactant administration using the advanced LISA method (Less Invasive Surfactant Administration) while maintaining non-invasive ventilation, thus reducing the unpleasant effects on the tiny baby. This LISA method is gradually replacing the traumatic antecedent procedures using an endotracheal tube and INSURE method.
We will dive deeper into the different surfactant administration strategies in the subsequent blogs.
For More Information Click here
For queries and/or demonstration, contact Click here
*******************************************************************************************************
References: –
[1] “How Your Lungs Get the Job Done” (2017, July 20), Each Breath by American Lung Association, retrieved from https://www.lung.org/blog/how-your-lungs-work
[2] Ochs, Matthias et al. “The number of alveoli in the human lung.” American journal of respiratory and critical care medicine vol. 169,1 (2004): 120-4. doi:10.1164/rccm.200308-1107OC
[3] M Hussain, C Xu et al., “Wnt/β-catenin signaling links embryonic lung development and asthmatic airway remodeling”, Biochimica et Biophysica Acta (BBA) – Molecular Basis of Disease, Volume 1863, Issue 12 (2017) https://doi.org/10.1016/j.bbadis.2017.08.031
[4] Turunen, Riikka, “Systemic Inflammation in Preterm Infants.”, Research Gate, (2009) https://www.researchgate.net/publication/47933972_Systemic_Inflammation_in_Preterm_Infants#pf31
[5] David G. Sweet et al., European Consensus Guidelines on the Management of Respiratory Distress Syndrome – 2019 Update, Neonatology 2019;115:432-450. https://doi.org/10.1159/000499361
[6] Saigal S et al. “An overview of mortality and sequelae of preterm birth from infancy to adulthood” The Lancet, Volume 371, Issue 9608 (2008), https://doi.org/10.1016/S0140-6736(08)60136-1.
[7] Engle, William A. “Surfactant-replacement therapy for respiratory distress in the preterm and term neonate.” Pediatrics 121.2 (2008): 419-432. https://doi.org/10.1542/peds.2007-3283








